

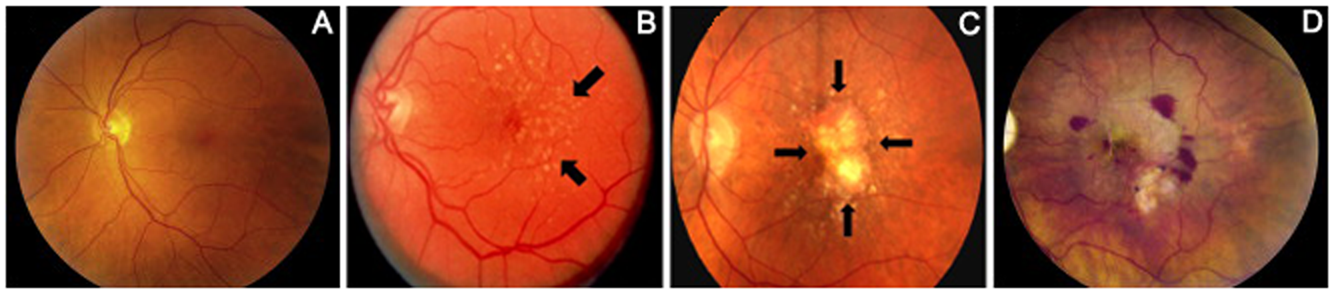
این بیماری ممکن است منجر به بروز احساس وجود خارجی در یک یا هر دو چشم شده ، به گونه ای که خود فرد احساس می کند قادر به بیرون آوردن جسم خارجی نیست، زمانی که فرد از خواب بیدار می شود، ممکن است چشم وی پر از ترشحات باشد. سفیدی چشم نیز به نظر قرمز آمده و فرد منظره ای را می بیند که قبلاً در چشم وجود نداشته است.
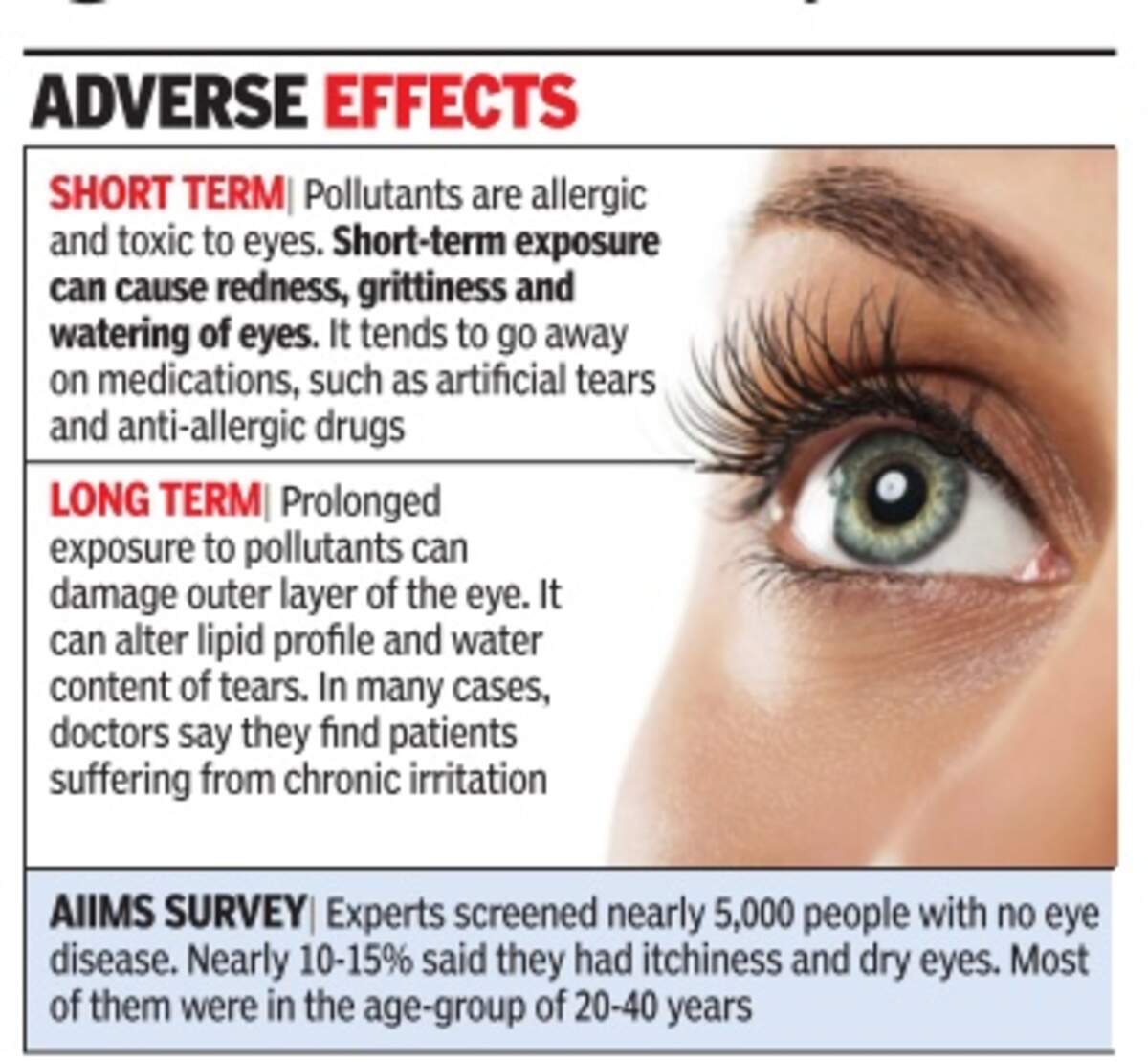
وجود التهاب سبب می شود که عروق کره چشم در مقایسه با قبل بیشتر مشخص شوند و همین عامل سبب می شود که سفیدی چشم به نظر قرمز رسد.قرمزی چشم اصطلاحی است که معمولاً برای بیان وجود التهاب ملتحمه به کار می رود.
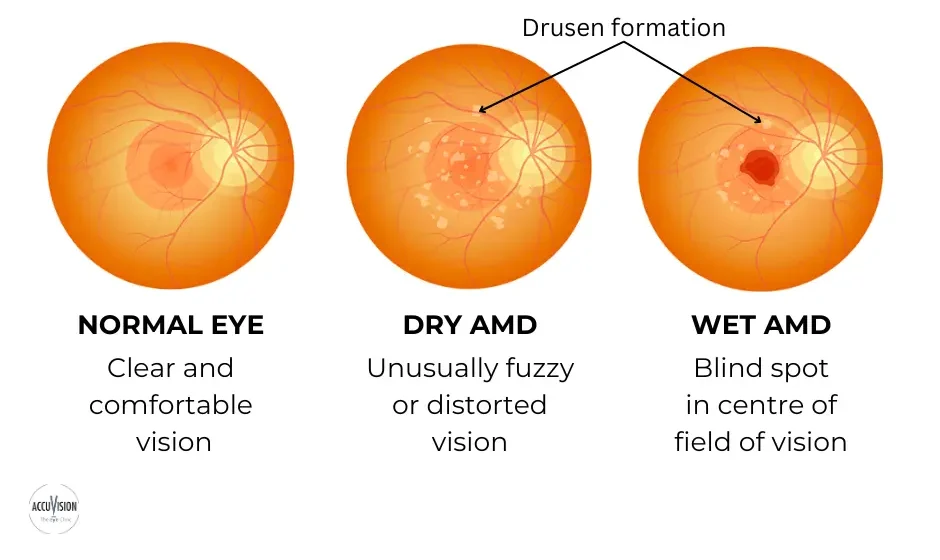
بنظر می رسد که بروز التهاب علاوه بر ایجاد قرمزی برروی بینایی نیز گاهی تأثیر می گذارد.اگر فردی دچار قرمزی چشم شد با انجام اقدامات خاصی می تواند شکایات خود را برطرف نماید.ولی از آنجایی که قرمزی چشم می تواند مسری باشد، لذا باید هرچه سریعتر تحت درمان قرار گیرد.این درمان سریع بخصوص در سنین قبل از مدرسه که کودک می تواند به التهاب ملتحمه باکتریایی یا ویروسی مبتلا شود بسیار مهم است.
علائم و نشانه ها
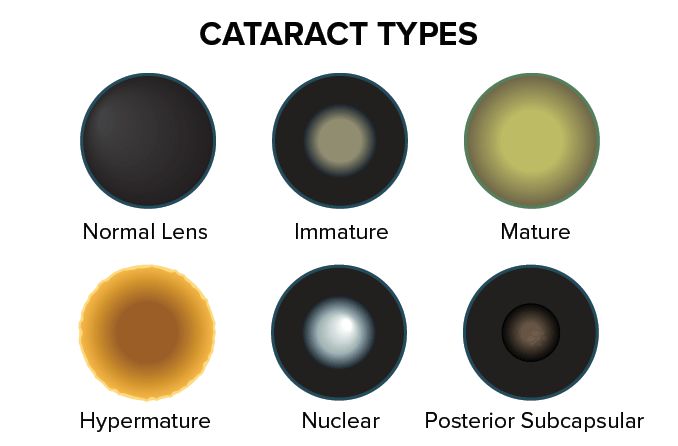
شایعترین علائم و نشانه های قرمزی چشم شامل خارش و یا قرمزی در یک یا هر دو چشم ، تاری دید و حساسیت به نور، وجود انواع ترشحات در یک یا هر دو چشم است که در طی شب منجر به تشکیل دلمه در چشم ها می شود و نهایتاً فرسودگی چشم خواهد بود.
علل
باکتریها،ویروسها و حساسیت می توانند منجر به بروز قرمزی چشم شوند اما شایعترین علت ویروسها می باشند. گاهی اوقات نوزادان ثانویه به عدم باز شدن کامل مجرای اشکی نیز
می توانند مبتلا به قرمزی چشم شوند.در ورم ملتحمه باکتریایی یا ویروسی، معمولاً یک یا هر دو چشم مبتلا می شوند این دو فرم باکتریایی و ویروسی می توانند با سرماخوردگی ارتباط داشته باشند، و هر دو فرم بسیار مسری هستند. این فرمها معمولاً در اطفال شایعتر بوده، اما بالغین نیز به همان نسبت می توانند مبتلا شوند.
در ورم ملتحمه حساسیتی معمولاً هر دو چشم مبتلا می شوند و معمولاً ثانویه به مواد حساسیت زا نظیر گرده گلها ایجاد می شود. در پاسخ به مواد حساسیت زا بدن شروع به ساختن موادی میکند که ایمنوگلوبولین E نام دارند . این مواد سبب تحریک سلولهای انتهایی شده و منجر به ترشح مواد دیگری گشته که آنجا موجب بروز به التهاب میشوند . از جمله این مواد هیستامین است. که آزاد شدن هیستامین در بدن میتواند منجر به بروز علائم حساسیت، نظیر قرمزی چشم ها شود. فرد مبتلا به قرمزی چشم حساسیتی ممکن دچار خارش شدید چشم ها شـود و علائم دیگری نظیر خارش بدن ، عطسه و ترشحات آبکی از بینی پیدا کند، بعلاوه ممکن است پلکها تا حدی دچار تورم شوند .
فاکتورهای خطر :
عوامل خطر که شاخص ابتلا را افزایش میدهند شامل تماس با مواد حساسیت زا و به همان میزان تماس با فردی که مبتلا به ورم ملتحمه باکتریائی یا ویروسی شده است میباشد . فرمهای ویروسی و باکتریایی معمولاً بسیار مسری بوده و فرد مبتلا میتواند تا 7 الی 14 روز بعد از شروع علائم سبب سرایت بیماری به دیگران شود .
چه زمانی باید به پزشک مراجعه نمود ؟
قرمزی چشم یک حساسیت تحریک کننده بوده اما در اکثر مواقع برای بینایی بی ضرر است و به ندرت نیاز به درمان فوری و شدید پیدا می کند. ولی از آنجایی که این بیماری می تواند تا 2 هفته بعد از شروع علائم مسری باشد لذا تشخیص و درمان به موقع بسیار مهم می باشد. کودکان مبتلا به ورم ملتحمه باکتریایی باید تا شروع درمان از سایر کودکان دور نگه داشته شوند. اما فرم ویروسی تنها تا چند روز مسری هستند. اگر مشکلی در ارتباط با زمان بازگشت کودک خود به مدرسه دارید حتماً با پزشک در میان گذارید. گاهی اوقات ورم ملتحمه سبب بروز عوارضی در قرنیه می شود که همین امر نیاز به درمان به موقع را مسجل می سازد.
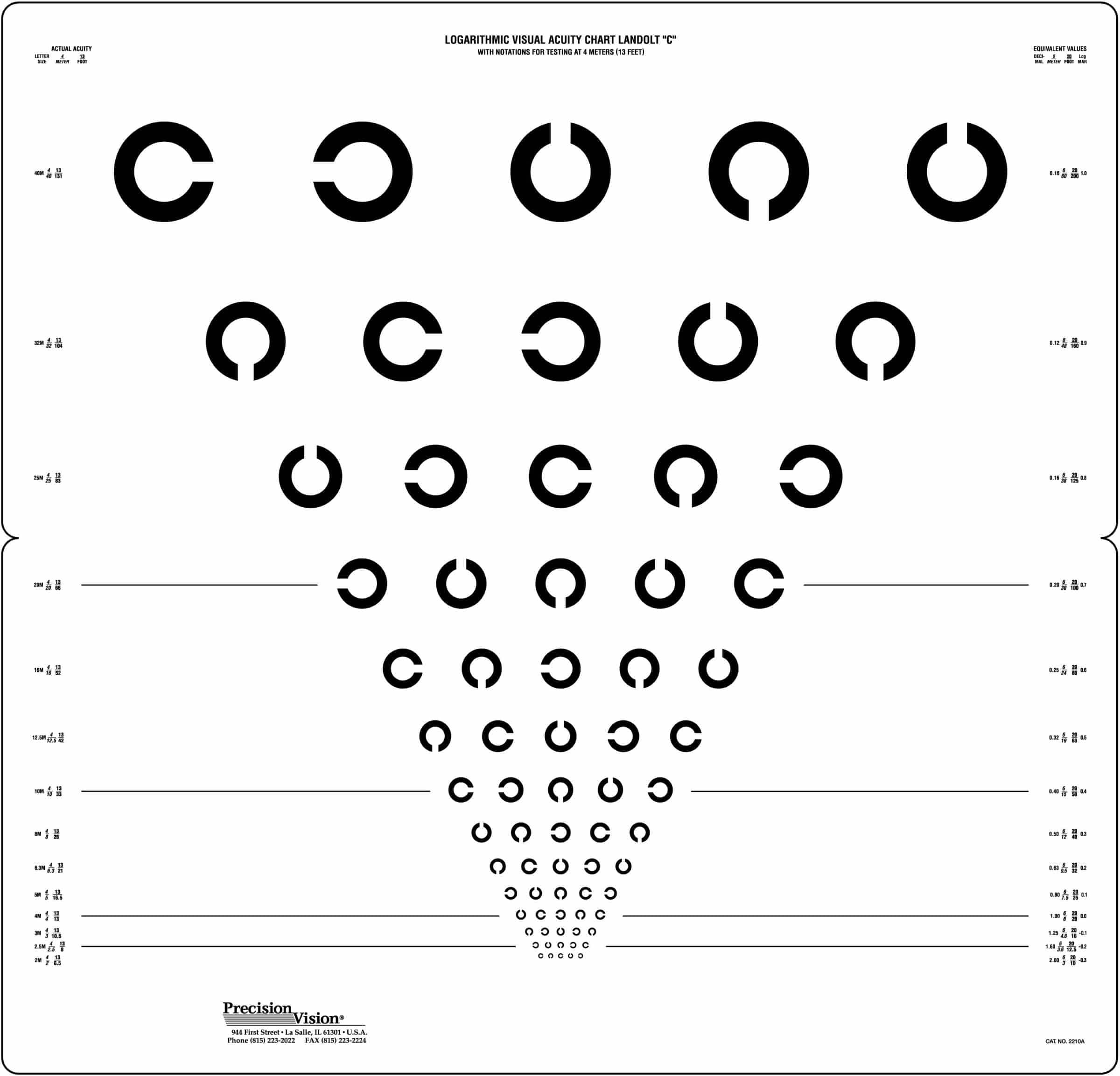
غربالگری و تشخیص
برای تشخیص عامل بیماری ممکن است پزشک از ترشحات نمونه ای تهیه کرده و به آزمایشگاه بفرست تا بدین ترتیب عامل بیماری مشخص شده و درمان بهتری صورت گیرد. اگر بیمار کودکی باشد که مرتباً دچار قرمزی چشم می شود. باید از نظر وجود انسداد در مجاری اشکی توسط پزشک مورد معاینه و ارزیابی قرار گیرد.
درمان
اگر عفونت باکتریایی وجود داشته باشد نیاز به استفاده از قطره های آنتی بیوتیکی بوده تا حد ممکن عفونت هر چه سریعتر درمان یابد. به منظور پیشگیری از عود عفونت باید دوره درمان بطور کامل طی شود. معمولاً عفونتهای ویروسی نیز به خودی خود در طی یک هفته درمان می شوند. اگر فرم حساسیتی وجود داشته باشد، ممکن است از انواع قطره های چشمی جهت درمان استفاده شود که شامل آنتی هیستامین ها، ضد اختقانها، کورتونها و قطره های ضدالتهابی می باشند.
پیشگیری
داشتن یک وضعیت بهداشتی خوب بهترین راه کنترل قرمزی چشم است .
زمانی که عفونت تشخیص داده شد باید اقدامات ذیل انجام شود.
-
هرگز با دست خود چشمهایتان را نمالید.
-
هر زمان که ممکن است و بصورت مکرر دستهای خود را بشویید.
-
هر روز حوله ها و لباسهای خود را بشویید و اجازه ندهید کسی دیگری از آنها استفاده کند.
-
وسایل آرایشی چشم های خود را دور اندازید و به کسی دیگر اجازه ندهید که از آنها استفاده کند و هرگز به دیگران اجازه ندهید که از وسایلی که با چشم های شما تماس داشته اند، استفاده کنند.
-
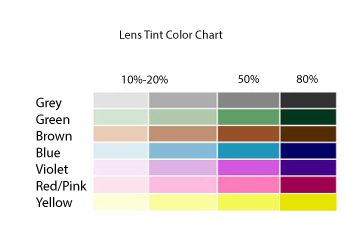
به توصیه های پزشک خود در ارتباط با نحوه محافظت از لنزهای تماسی چشم خود عمل نمایید.
اگر کودکتان مبتلا به قرمزی چشم بوده و یا قرمزی چشم در مدرسه آنها شیوع پیدا کرده است از تماس آنها با سایرین ممانعت کنید. بسیاری از مدارس کودکان مبتلا را به خانه می فرستند.
نوزادان بسیار مستعد ابتلا به عفونتهای چشمی باکتریایی موجود در کانال زایمان هستند. این باکتریها در مادر هیچگونه علامتی ایجاد نمی کنند.گاهی اوقات این باکتریها در نوزادان منجر به بروز عفونتهای چشمی بسیار شدیدی می شوند که نیاز به درمان فوری دارند. وجود همین اختلال سبب شده است که بلافاصله بعد از تولد از قطره های آنتی بیوتیکی چشمی نظیر اریترومایسین استفاده شود.
مراقبت از خود
فرد می تواند با استفاده از کمپرسهای گرم برروی چشم مبتلا از شدت علائم آن بکاهد. بدین منظور از یک پارچه تمیز استفاده نموده و آنرا بعد از قرار دادن در آب ولرم و فشردن آن ، آنرا به آرامی بر روی چشم های خود قرار دهید.
در موارد حساسیتی از مالیدن چشم هایتان خودداری ممانعت کنید، چرا که سبب رها شدن بیشتر هیستامین خواهد شد،در عوض می توان از کمپرس سرد برای تسکین علائم استفاده نمود. در این موارد از قطره های چشمی آنتی هیستامین و منقبض کننده های عروقی استفاده نمائید.
منبع: مركز پژوهش هاي سلامت خليج فارس www.pghrc.ir



:max_bytes(150000):strip_icc():format(webp)/top-causes-of-red-eye-3422111-5c04703446e0fb0001bbec58.png)























































































 وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.
وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.