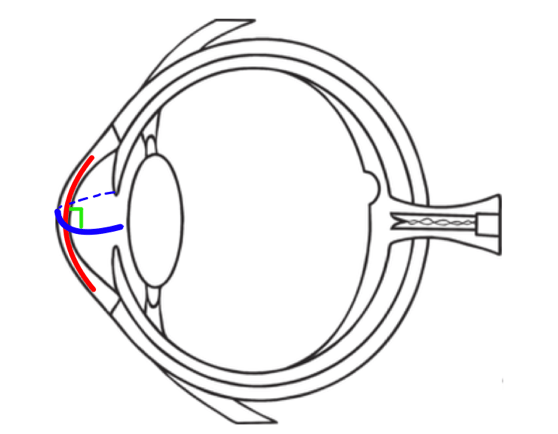
Glasses and contact lens prescriptions with regular astigmatism have two different power numbers, one for each curve in order to focus light together instead of in two separate spots. Unfortunately, prescriptions can only be written for regular astigmatism. Irregular astigmatism is when the two different curves are not perpendicular to each other(blue and red lines, Figure below).
Due to this irregularity, contact lenses need to be personalized to match these curves.
The terms irregular and regular astigmatism are used to describe the curvature of the eye, not necessarily the health of the eye. The eye can have either type of astigmatism and still be considered healthy.
What Causes Irregular Astigmatism?
Not all causes of irregular astigmatism are known, but eye care experts have linked it to systemic and ocular diseases and conditions that cause the cornea to warp or thin, injuries from sports or work, and procedures such as LASIK and other types of vision correction surgery.
Causes of Irregular Astigmatism
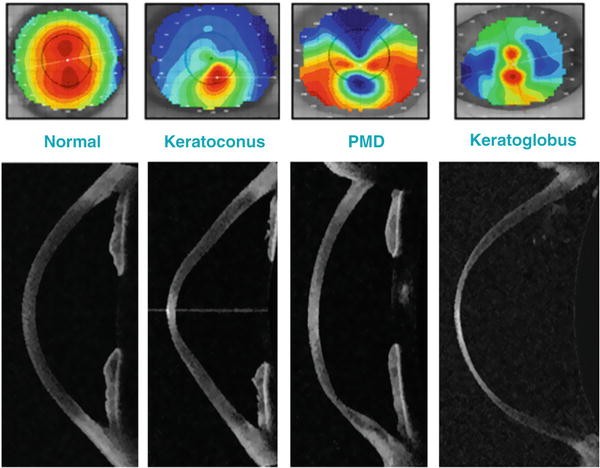
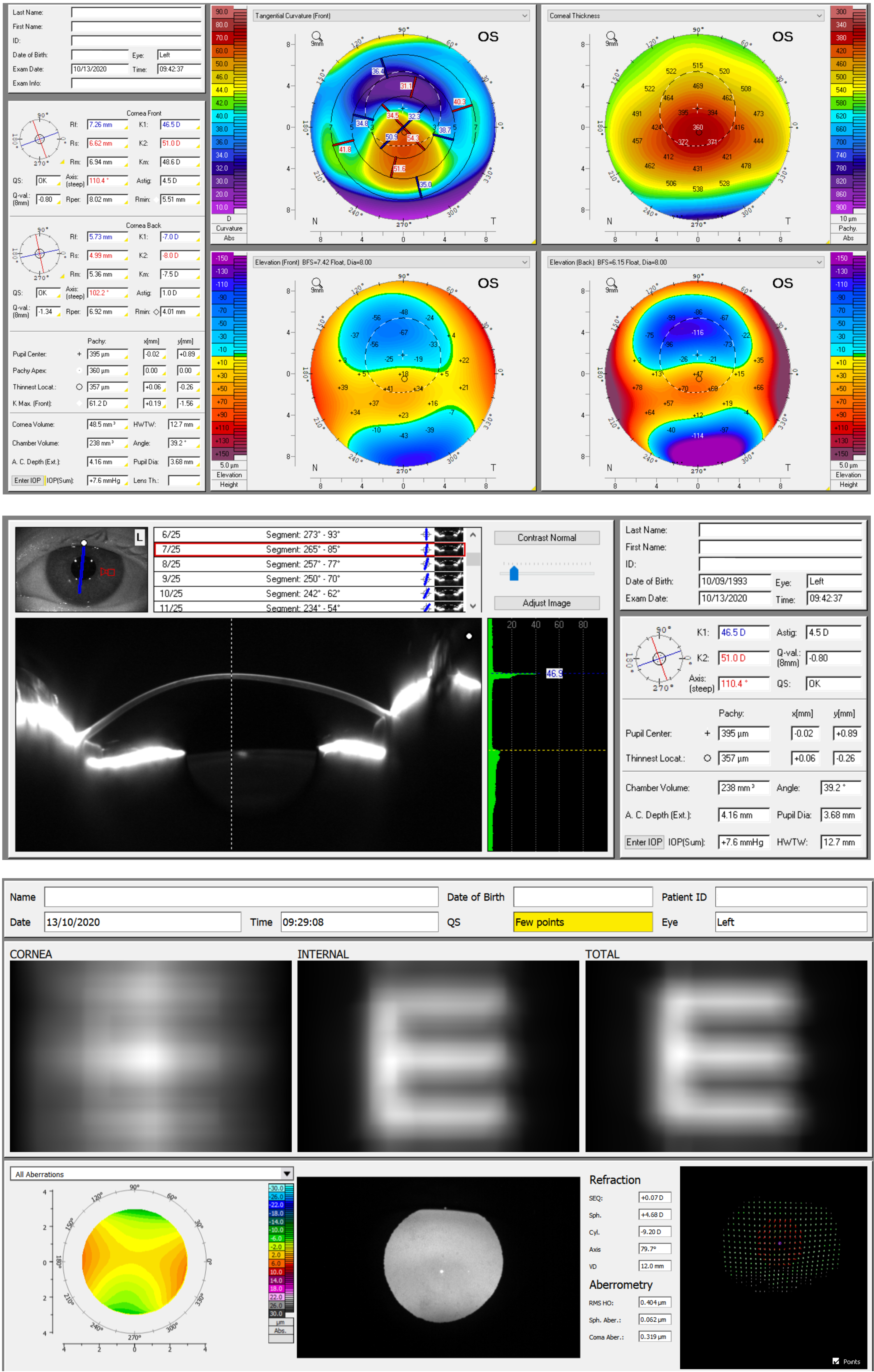
- Keratoconus: This condition thins and weakens the central cornea until the age of 30-40, causing it to bulge outwards. This thinning causes the cornea to go from being rounded and smooth to being pointed, creating a cone-like shape, and making the corneal surface uneven.
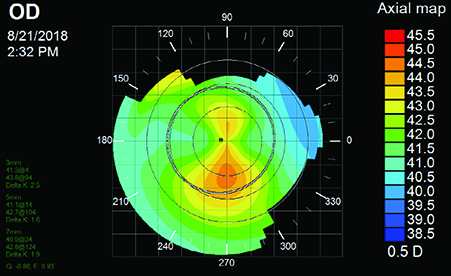
- Pellucid marginal degeneration (PMD): This condition is very similar to keratoconus, except that it continues throughout life. Specifically, the lower third of the cornea continues to thin and weaken. This creates a protrusion at the bottom, resembling a belly shape.
- Keratoglobus: This condition is also similar to keratoconus, except that the cornea thins and weakens in the periphery creating a very rounded bulging ‘globe’ appearance.
- Trauma to the eye: A deep cut or tear, stitches, or warpage from a previous contact lens fitting too tight can change the curves on the cornea.

Pellucid Marginal Degeneration vs. Keratoconus - Corneal surgery: Corneal transplant/partial corneal tissue replacements and refractive surgeries can lead to complicationsof changing curves on a cornea.
A list of procedures are as follows:
-DALK (Deep anterior lamellar keratoplasty)
-PKP (Penetrating keratoplasty)
-RK (Radial keratotomy)
-PRK (Photorefractive keratectomy)
-LASIK (Laser in-situ keratomileusis)
As mentioned above, pellucid marginal degeneration (PMD) is a corneal disease and a rare form of corneal ectasia (a group of disorders that cause the cornea to thin and protrude outward).
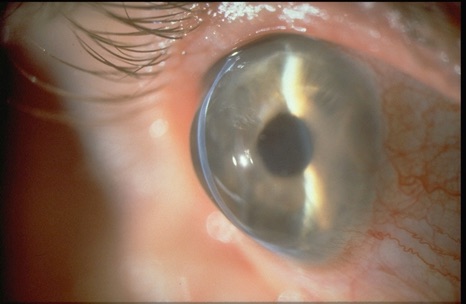
Normally, a healthy and thick cornea enables the eyes to see clearly. However, in PMD, the cornea thins over time. This thinning typically occurs in the lower part of the cornea, extending from the 4 o'clock to 8 o'clock position. Above the thinned area, the cornea protrudes outward. These changes in the cornea can lead to astigmatism and a gradual decline in visual acuity.
PMD usually affects both eyes, although it may occur in only one eye in some cases. This condition does not cause scarring in the eyes, allowing the cornea to remain transparent. For reference, the term "pellucid" means clear or transparent.
To date, experts have not yet determined the exact cause or risk factors for developing pellucid marginal degeneration (PMD). However, PMD is more commonly diagnosed when one is in their 20s, 30s, or 40s. While it can also be diagnosed when an individual is in their 50s or older, such cases are rare. So far, there is no scientific evidence suggesting that PMD is hereditary. However, some patients diagnosed with PMD have been recorded to have family members with moderate to severe astigmatism. eResearch by Navid Ajamin -- winter 2025
Treatment
Eye glasses
Most patients can be treated non-surgically with eye glasses, or contact lenses.
Contact lenses
Early stages of PMD may also be managed with soft contact lenses. Success has been shown with the use of rigid contact lenses combined with over-refraction. Patients wearing contacts report increased problems with glare and contrast sensitivity, but it is not clear if this is due to the corneal disease, or the contact lenses themselves.
New studies show that the use of a "GP" or Scleral contact lens has shown promise for most patients that exhibit Pellucid Marginal Degeneration. Most of these lenses are in the range of 15.5mm to 18.0mm in diameter.
Regardless of the lens size, it is thought that the larger the GP lens, regardless of the fact that it is a rigid lens, will in most cases be more comfortable then standard rigid corneal lenses, and at times more comfortable than soft lenses.
The highlight to the scleral design and the correction of eye disorders such as Pellucid Marginal Degeneration is that vision with these types of lenses is exceptional when fit correctly.
Intacs
The use of intacs implants has been tested as a treatment for PMD, with slight improvement in visual acuity noted after eleven months,and intacs have been used with keratoconus with success.
Collagen Cross Linking
There is evidence suggesting corneal collagen cross-linking may be beneficial for patients with pellucid marginal degeneration.
Surgery
Corneal transplant surgery may be difficult due to the peripheral thinning of the cornea, even with large and off-center grafts. Therefore, surgery is usually reserved for patients that do not tolerate contact lenses.
Several different surgical approaches may be taken, and no one approach is currently established as the standard.
Examples of surgical procedures used for PMD include: wedge resection, lamellar crescentic resection, penetrating keratoplasty, lamellar keratoplasty, epikeratoplasty and intracorneal segments.
Transplantation of the entire thickness of the cornea (penetrating keratoplasty) may be performed if there is enough normal tissue present. However, if there is not enough normal tissue present, then attaching the graft is difficult.
Due to the thinning of the cornea, PMD patients are poor candidates for procedures such as LASIK and photorefractive keratectomy.
Epidemiology
The incidence and prevalence of PMD are unknown, and no studies have yet investigated its prevalence or incidence. However, it is generally agreed that PMD is a very rare condition. Some uncertainty regarding the incidence of PMD may be attributed to its confusion with keratoconus. PMD is not linked to race or age, although most cases present early in life, between 20 and 40 years of age. While PMD is usually considered to affect men and women equally, some studies suggest that it may affect men more frequently.
Several diseases have been observed in patients with PMD. However, no causal relationships have been established between the any of the associated diseases and the pathogenesis of PMD. Such diseases include: chronic open-angle glaucoma, retinitis pigmentosa, retinal lattice degeneration, scleroderma, kerato-conjunctivitis, eczema, and hyperthyroidism.
Prognosis
Visual function declines as a result of the irregular corneal shape, resulting in astigmatism, and causing a distortion in vision. Deterioration can become severe over time.

Reference:
- researchgate.net/figure/Corneal-thickness-map-of-a-true-case-of-pellucid-marginal-degeneration-The-pachymetric_fig2_255706001
- drbrendancronin.com.au/blog/pellucid-marginal-degeneration-vs-keratoconus-understanding-the-similarities-and-differences
- siloamhospitals.com/en/informasi-siloam/artikel/understanding-pellucid-marginal-degeneration
- oogziekenhuis.me/Keratoconus/Pellucide_marginale_degeneratie.html
- clinevada.com/irregular-astigmatism





 وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.
وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.