Did you know that an error of only 2mm can lead to a loss of more than 40% of your clear vision field?
What happens if you get your PD wrong?
Reduced Depth Perception: An incorrect PD can affect your depth perception, making it difficult to judge distances accurately. Adjustment Issues: You might find it hard to adjust to the glasses, leading to frustration and possibly abandoning their use altogether.
Ensuring the accuracy of your pupillary distance (PD) is crucial when it comes to ordering prescription glasses. If you enter incorrect prescription information, including an inaccurate pupillary distance measurement, the consequences could affect your vision with the new glasses.
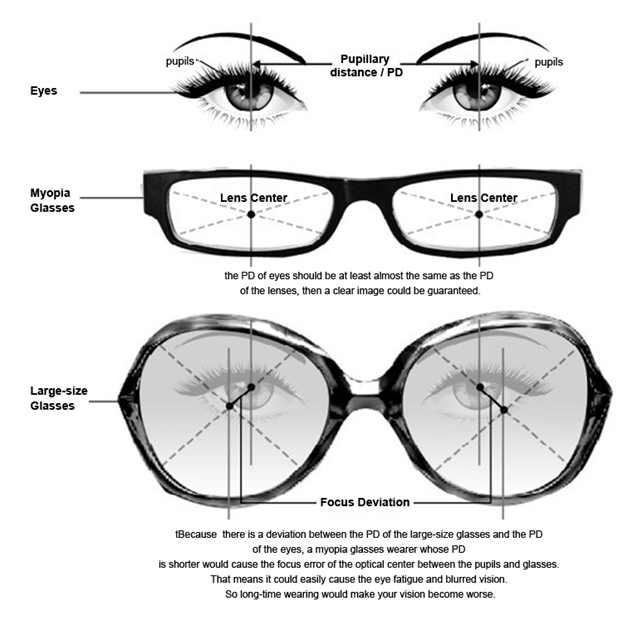
PD, or pupillary distance, refers to the distance in millimeters between the center of one pupil to the center of the other. It is used to determine where the optical center of the lens should be placed on your glasses that need to line up over the center of the pupil. Having a correct measurement of your PD on your glasses prescription ensures that you’re looking through the ideal precise placement spot (Optical Center) in your lenses.

Mean IPD in adult subjects was 61.1±3.5 mm in women and 63.6±3.9 mm in men (p<0.001). Mean IPD increased 4.8 mm during the second decade, 1.7 mm during the third decade, and 0.6 mm during the fourth and fifth decades of life.
There are two types of pupillary distance measurements:
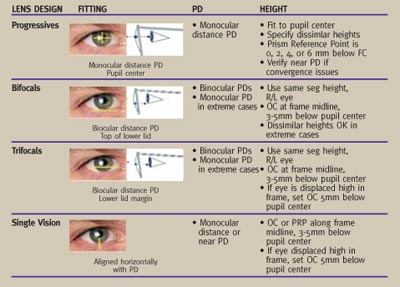
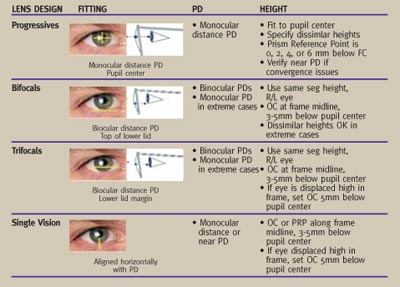
Monocular PD. This is the distance between the center of your pupil and the middle of the bridge of your nose. Monocular PDs are required for accurate fitting of progressive lenses.
Binocular PD. This is the distance between the center of the pupil of one eye and the center of the pupil of the other eye.
There are two ways to measure the distance: single PD and dual PD.
Single PD will measure the distance between the center of one pupil to the other while dual PD consists of two numbers and is the distance between the centers of each pupil to the bridge of the nose.
For Example, The average adult's single PD is between 54-74 mm; kids' are between 43-58 mm but a fun fact is that most of us are not symmetrical and therefore your dual PD will be most likely not even 32/30.

What is the tolerance for PD?
While the PD tool is consistent up to ±1 mm for 95% of the scans, the PD tolerance in the industry is up to ±2.5 mm, which means you are good to go with any single result from the PD scan. ** No results should be obtained within ±2.5 mm or higher from each other, if the card was held properly flat against the forehead.
What is standard PD?

What is a normal pupillary distance? The average pupillary distance of a typical adult ranges from 54 to 74 mm without much difference between the average female and male PD. A child's distance ranges from 43 to 58 mm. During an eye checkup, your optometrist will typically measure your PD.
Misaligned glasses put extra load on your eye muscles, forcing them to work harder to bring objects into focus. This may cause migraines, eyestrain, and discomfort. Prolonged eye muscle strain may cause more serious eye defects like asthenopia—eye fatigue.
Pupillary Distance (PD), also known as interpupillary distance, is the horizontal distance between the centres of your pupils—the dark circle in your eye that shrinks to focus near objects and widens to accommodate light from far objects. PD is measured in millimetres.
The PD value is used to properly align your glasses with your eyes. Wearing misaligned glasses may cause side effects like eye strain, nausea, and distorted vision. Your PD value doesn’t appear on your prescription; as a result, you have to take this measurement yourself to be able to order your glasses from us.


Benefits of Accurate PD Values
An accurate PD measurement helps us align your lenses to fit your eyes perfectly. Here are some of the benefits of wearing properly aligned glasses:
- + Properly aligned lenses give you the best possible clarity and definition.
- + They provide you with comfort and reduce headaches and eyestrain by making sure that your eye muscles do not do more work than necessary.
- + Properly aligned glasses give you an accurate perception of depth and distance, helping you perform tasks like driving and walking safely.
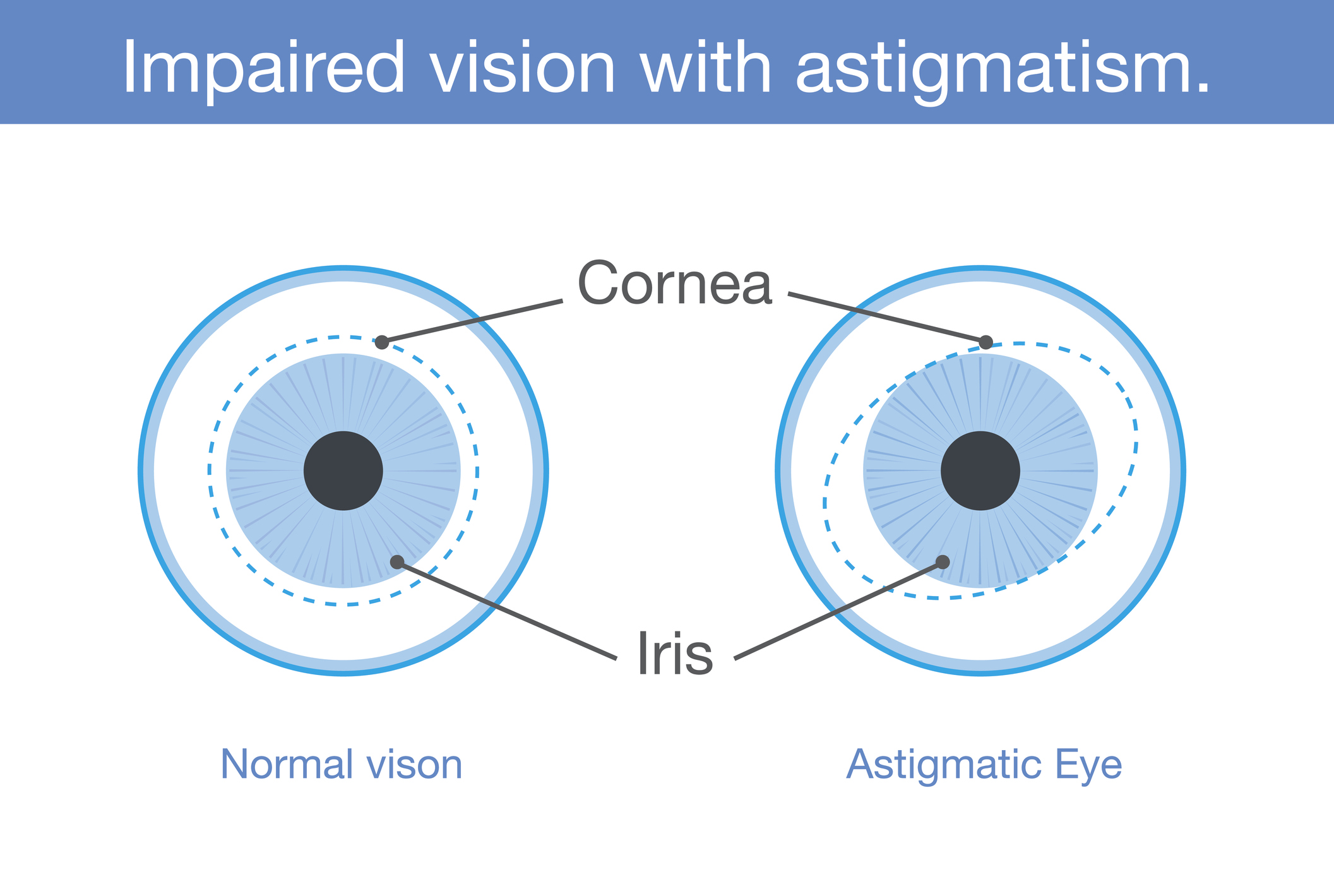
- + Properly aligned glasses make sure that the corrective power of your lens is applied accurately, with the right power and at the right angle/axis. This is particularly important for cylindrical lenses and astigmatism correction.
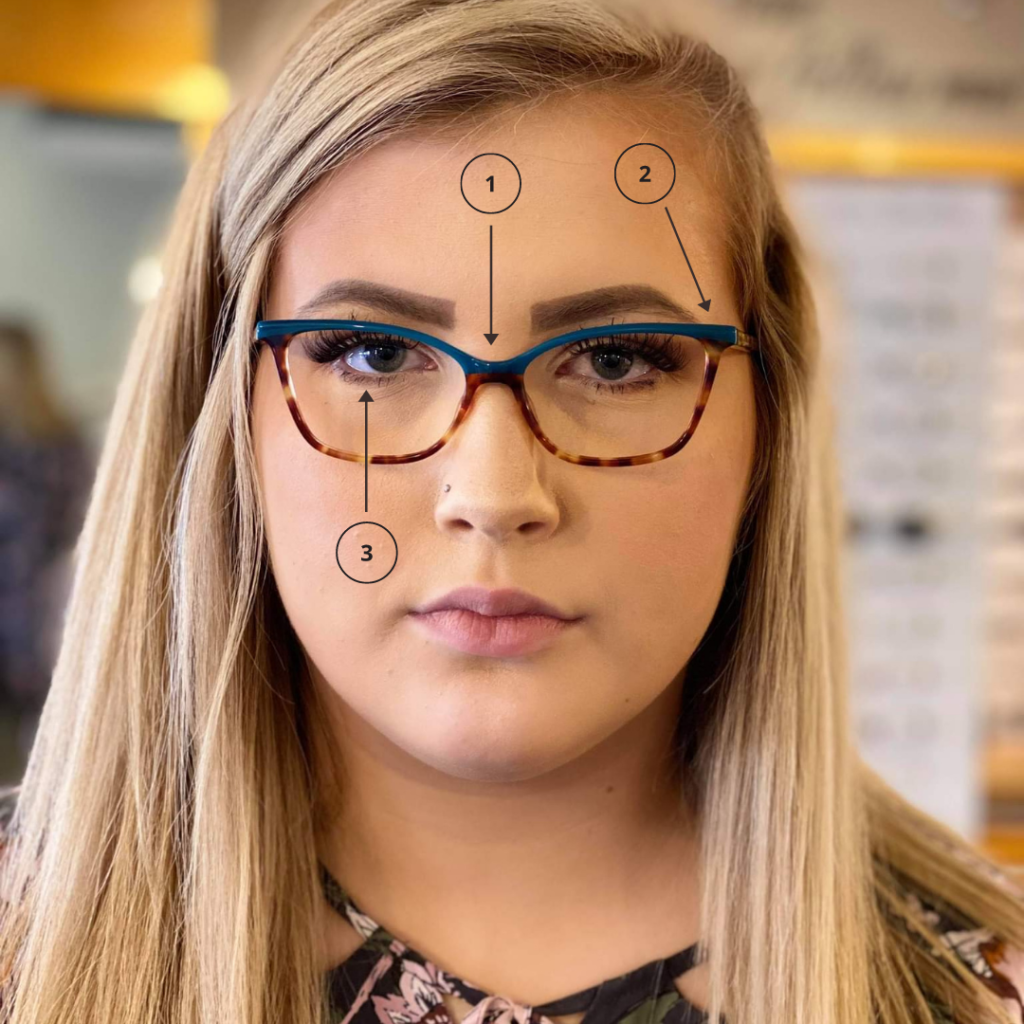
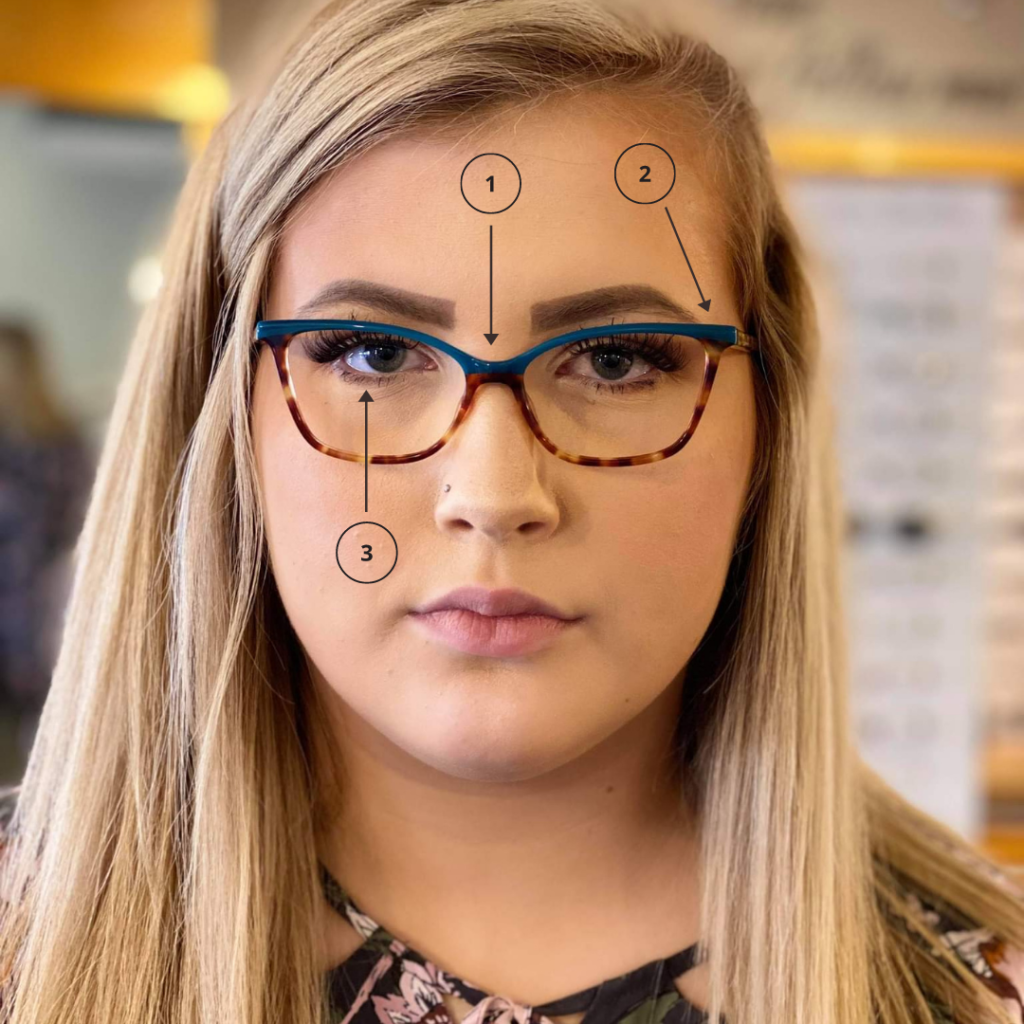
- The bridge is narrow
- The frame ends before the wearer’s temples – and sits too close to the side of the wearer’s head
- The eyes are not centered in the frame – they are sitting too high
Side Effects of Wrong PD Values
Entering the wrong PD value while ordering your eyeglasses will unfortunately lead to you receiving misaligned glasses. The list below includes a few of the side effects of wearing misaligned glasses:
- - Misaligned glasses put extra load on your eye muscles, forcing them to work harder to bring objects into focus. This may cause migraines, eyestrain, and discomfort. Prolonged eye muscle strain may cause more serious eye defects like asthenopia—eye fatigue
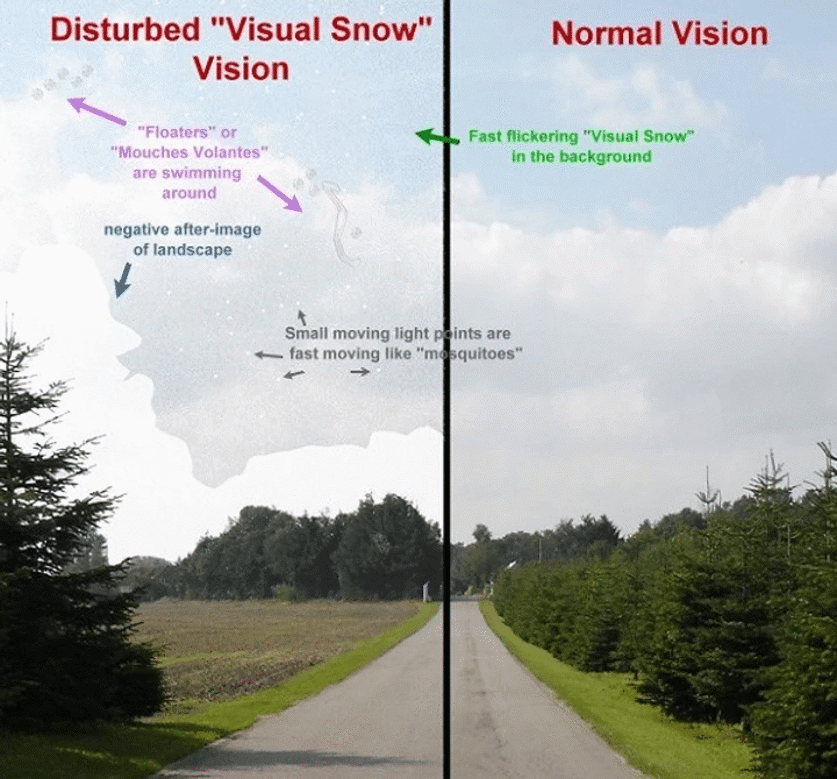
- - Improper lens alignment may cause blurred or double vision, making basic tasks, like reading more difficult.
- - Misaligned lenses also give a false sense of depth and distance, making it harder to drive or walk. This may even lead to an increased risk of accidents.
- - They may further weaken the ability of the eyes to focus, worsening eye defects in the process. This is why we often advise not to wear other people’s prescribed glasses.
How do you calculate near PD for reading glasses?
Subtract 3 mm from your distance PD. For example, if your distance PD is 63mm, then your near PD is 60mm. If you use dual PD to calculate near PD, then subtract 1.5mm from each eye's measurement.
Do I use dist PD or near PD when ordering progressive glasses?
If you need progressive or bifocal lenses, you'll also need to measure your near focus PD. You will need someone else to measure this for you to get the most accurate reading. The person measuring should follow the same instructions as they would to get your regular PD. eResearch by Navid Ajamin -- autumn 2024
Fitting glasses. For the best viewing experience, you want the center of your lens to sit right in front of your pupil. The center has the clearest part of your prescription, so lining it up with your pupil helps you see well and lowers eye strain. The measurement will change, though, depending on the type of glasses you buy.
An optician might use a handheld tool called a pupillometer or a digital PD meter. They hold this up to your face and adjust it to get the right distance. They might also use a special ruler to measure, or they might make marks on a pair of glasses and then measure the distance between them.
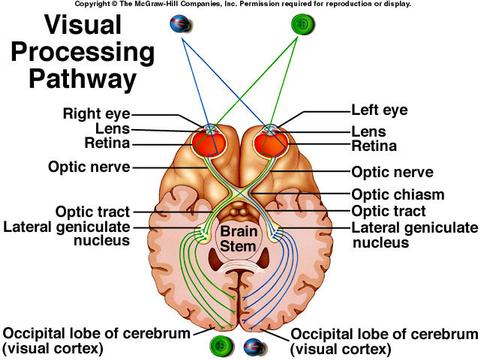
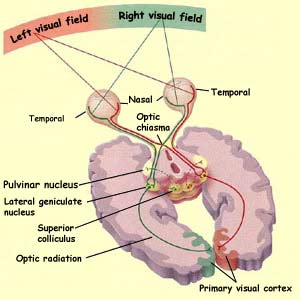
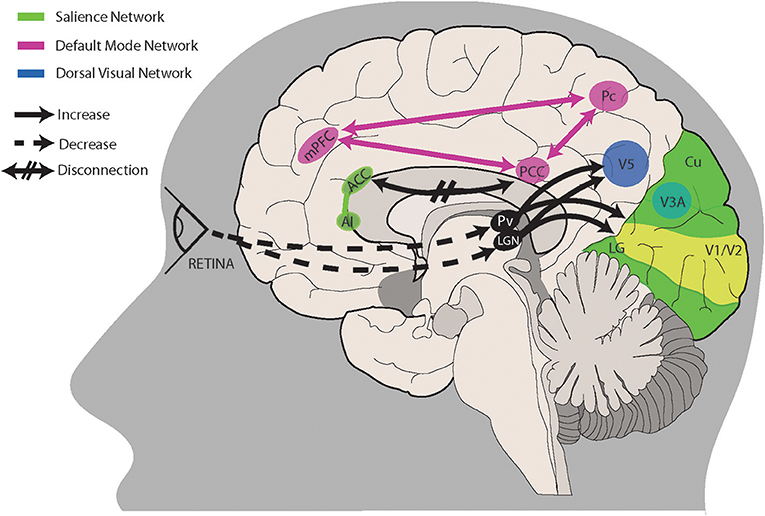
Testing stereo acuity. Your eye doctor will use PD to understand your stereo acuity, which is your depth perception. Both eyes see images and objects individually, but your brain puts those left and right visions together to form a three-dimensional image. The pupillary distance helps your doctor understand how much your field of vision differs between your left and right eyes.
Testing near-point convergence. Near-point convergence occurs when your eyes focus together on a nearby object. Your doctor might test this by bringing a pencil or other object toward your nose and watching how well your eyes come together to focus.
Your pupillary distance gets shorter as your eyes converge, or come together, so your doctor might check to see that your PD is changing.
The pupillary distance is especially important for fitting reading glasses.
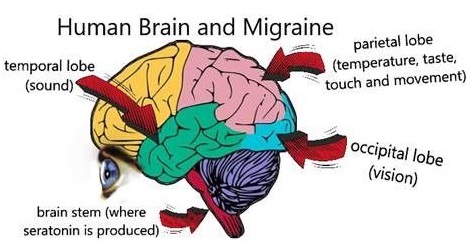
How The Wrong PD Will Give You Headaches
With the light bent “wrong” when arriving at your retinas while your PD isn’t right, things aren’t going well. The visual cortex in your brain is working overtime, trying to to “fix” the incorrect visual signal. Like your computer overheating when you tax the CPU with lots of computing, your brain is going to tell you that it’s not dealing well with this work – via fatigue and headaches.
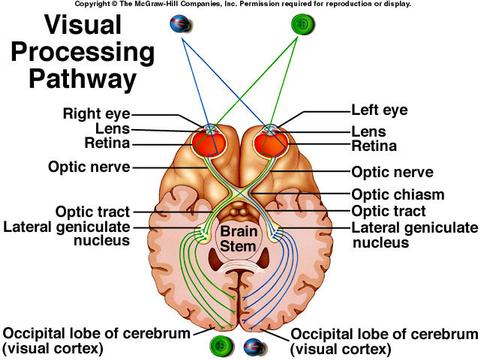 It’s important to remember that vision happens in your brain. So when things go wrong with the visual signal, it’s your headaches that are the most common result.
It’s important to remember that vision happens in your brain. So when things go wrong with the visual signal, it’s your headaches that are the most common result.
If you're wearing glasses made using an incorrect PD measurement, you'll probably notice symptoms related to the misalignment. Those include eyestrain, headaches and distortions in your vision. These symptoms aren't dangerous, but they also aren't pleasant.
What is the most common type of eye disorder?
Refractive errors are some of the most common eye conditions. They're also usually easier to treat, with corrective lenses like eyeglasses or contact lenses helping to adjust eyesight and improve visual acuity.

The top 25 common eye problems and their definitions are listed below.
- Glaucoma: Glaucoma is an eye condition that causes a loss of peripheral vision (visual field loss) through damage to the optic nerve.
- Cataracts: Cataracts form in the eye lens as a result of clumping of protein, leading to a decline in clear vision which commonly occurs naturally with advancing age.
- Uveitis: Uveitis refers to a group of conditions that causes eye inflammation and damages the uvea which is the middle layer of the eye.
- Dry eyes: Dry eye syndrome is caused by either the tears in the eyes evaporating too quickly or the eyes not producing enough tears.
- Presbyopia: Presbyopia is an age-related eye condition that occurs when the lens inside the eye becomes more rigid, becoming less able to focus clearly at near distances.
- Floaters: Floaters in the eye is a very common condition that usually occurs naturally with age and causes spots and lines to drift and float through a person’s vision.
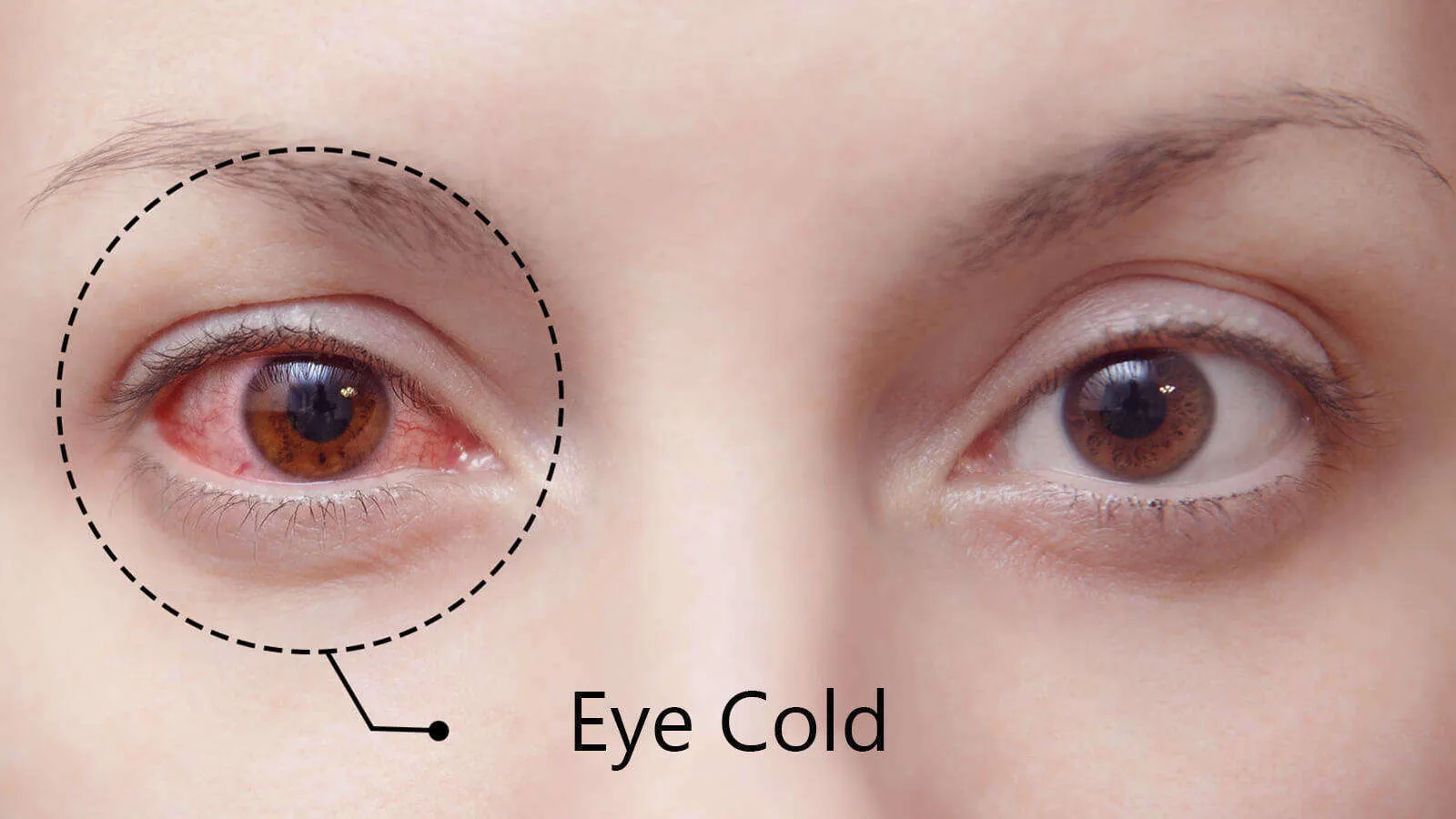
- Red eyes: Red eyes occur when the tiny blood vessels on the white part of the eye dilate, making the eye look more red than usual.
- Night blindness: Night blindness is an eye problem that impairs a person’s vision meaning they struggle to see in dim light or at night.
- Lazy eyes: Lazy eyes, also known as amblyopia, is an eye condition that describes a person with one eye that has weaker vision than the other.
- Colour blindness: Colour blindness is an eye condition that means a person is able to perceive colour but has trouble telling the difference between certain colours.
- Eyestrain: Eyestrain is a very common eye problem and is caused by the eyes concentrating on tasks or objects for a long period of time.
- Vision changes: Vision changes are a common sign of many eye conditions and are characterised by a sudden difference in your ability to see normally.
- Excess tearing: Excess tearing causes watery eyes due to the eyes producing too many tears or there being an issue with the film drainage of the eyes.
- Retinal disorders: Retinal disorders are a term for a group of conditions that affect the retina. Common retinal disorders and diseases include age-related macular degeneration and retinal tear and detachment.
- Eyelid problems: Eyelid problems are eye conditions that affect the eyelids, potentially making them swollen, painful and irritated.
- Corneal diseases: Corneal diseases are diseases that mainly affect the cornea. Some common corneal diseases include keratitis, eye herpes and pterygium.
- Problems with contact lenses: People may experience problems with contact lenses that can lead to certain eye conditions and symptoms.
- Cross eyes (strabismus) and nystagmus: Crossed eyes is an eye condition that occurs when one eye turns in a different direction than the other eye. Nystagmus causes involuntary movement of the eyes which can be side-to-side, circular or up and down.
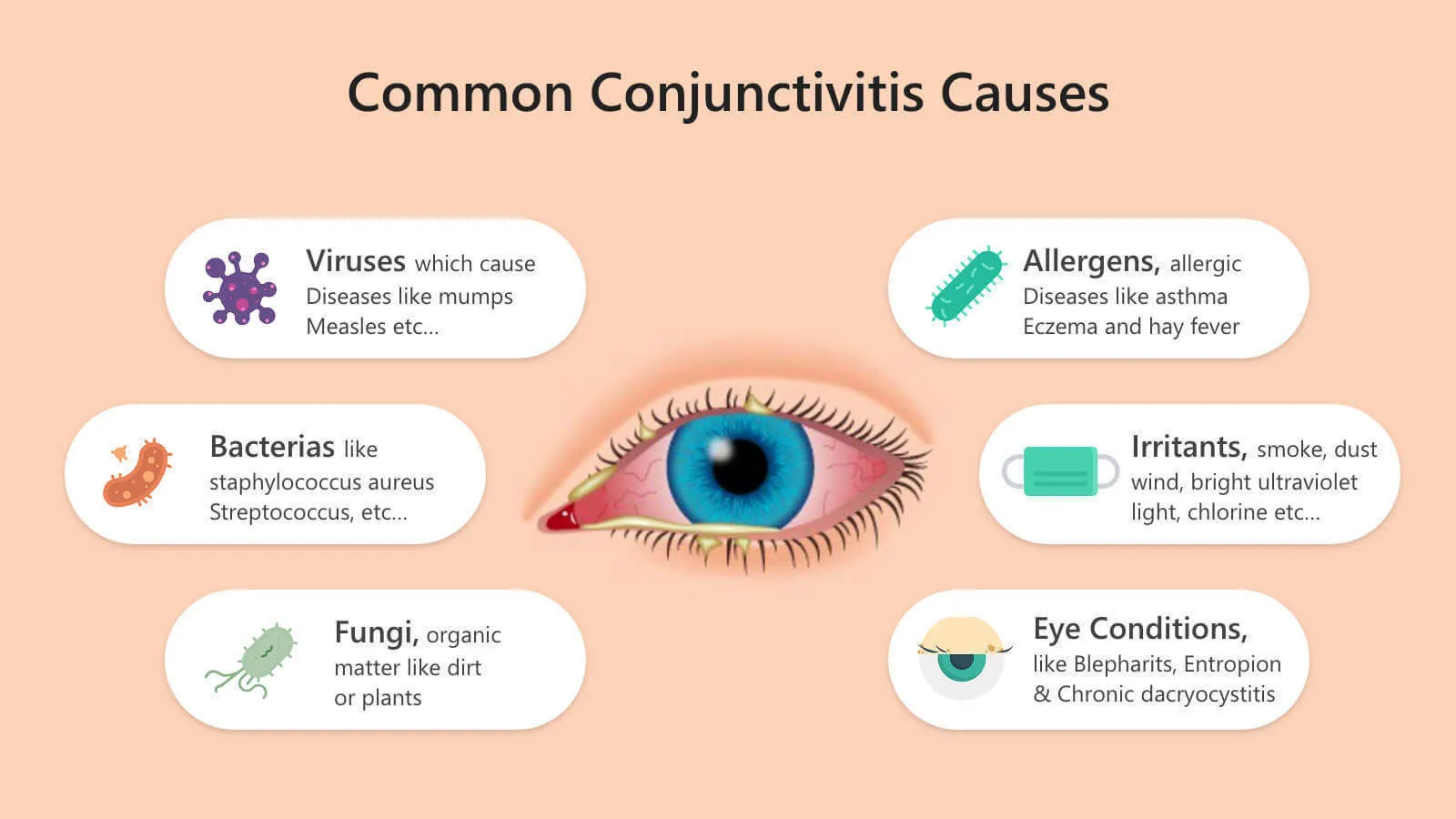
- Conjunctivitis (pink eye): Conjunctivitis is an inflammation of the conjunctiva, a lining covering the white part of the eye and underneath the eyelids.
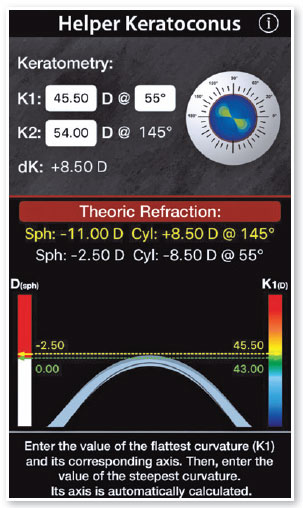
- Keratoconus: Keratoconus is an eye disease that affects the cornea, making it thin and bulge outwards.
- Chalazion (eyelid cyst): A chalazion is an eyelid cyst that is a sign of a blocked oil gland, usually underneath the upper eyelid, resulting in swelling of the affected area.
- Pterygium (noncancerous growth on the conjunctiva): Pterygium, also known as surfer’s eye, is a benign, noncancerous eye growth on the conjunctiva.
- Pinguecula (yellowish growth on the conjunctiva): A pinguecula is a yellow, raised growth on the conjunctiva that usually contains calcium, fat or protein.
- Diabetic retinopathy: Diabetic retinopathy is a complication of diabetes where the small blood vessels in the back of the eye are damaged.
- Age-related macular degeneration: Age-related macular degeneration is a common eye condition that causes a painless loss of central vision.
Reference:
- glasses.com
- docs.luna.io/docs/pd-reade
- webmd.com/eye-health/pupillary-distance
- zennioptical.com/measuring-pd-infographic
- lowcostglasses.co.uk/distance-pd-vs-near-pd
- oscarwylee.com.au/glasses/eye/common-problems
- eyebuydirect.com/guides/how-to-measure-your-pd
- endmyopia.org/how-to-measure-pd-pupillary-distance
- allaboutvision.com/eye-care/measure-pupillary-distance
- rx-safety.com/2014/02/does-pupillary-distance-have-to-be-exact
- researchgate.net/figure/Mean-interpupillary-distance-mm-values-in-various-age-groups
- finestglasses.com/landingpage/would-your-vision-become-worse-if-you-wear-large-sized-glasses-often.html
- visionsource-meadville.com/2021/09/03/answers-to-4-faqs-about-eyeglasses-to-help-you-find-the-perfect-fit
- eyecareleaders.net/blog/2023/6/9/what-is-pupillary-distance-pd-and-why-is-it-important-to-have-an-accurate-measurement-of-it
See also: Normal Interpupillary Distance Values in an Iranian Population























 It’s important to remember that vision happens in your brain. So when things go wrong with the visual signal, it’s your headaches that are the most common result.
It’s important to remember that vision happens in your brain. So when things go wrong with the visual signal, it’s your headaches that are the most common result.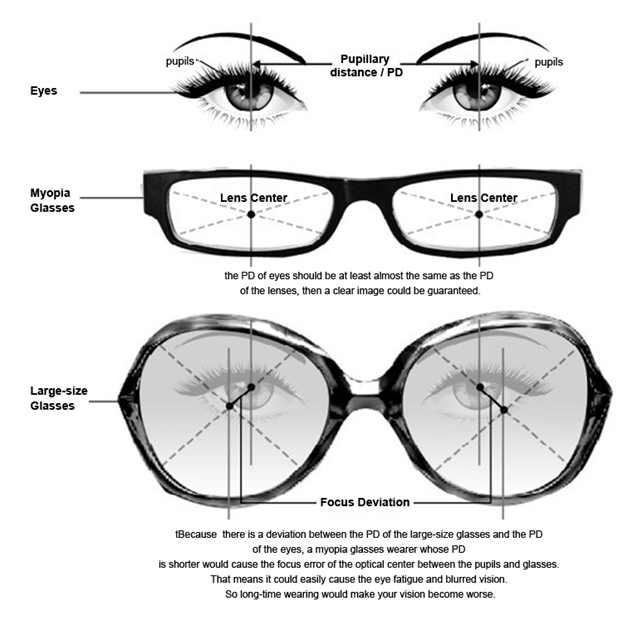











:max_bytes(150000):strip_icc():format(webp)/street-light-glare-b2a557dd487949c2b04216eb83f86800.jpg)








 وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.
وبلاگ تخصصی عینک شامل مجموعه مطالب پزشکی است که اطلاعات مفیدی در رابطه با عینک , چشم، لنز، سلامتی چشم و راه های پیشگیری از بیماریهای چشمی، کنترل و درمان آن را در اختیار شما کاربر محترم می گزارد.